This article is a collection of the best answers to Colorado Medicaid’s most frequently asked questions.
Medicaid is a government-sponsored healthcare program for low-income families and individuals who fulfill specific income and resource requirements. Only the aged, blind, or disabled can access resources within the defined restrictions.
We have scoured the internet to provide all you need to know about the Colorado Medicaid Benefits.
You will learn everything you need to know about Colorado Medicaid in this article.
Table of Contents
What is Colorado Medicaid?
Medicaid offers health coverage to millions of Americans including children, parents, seniors and people with disabilities. Some states offer the program to all low-income adults with incomes below a certain level.
Who is eligible for Colorado Medicaid?
You must be a resident of Kentucky, a national or citizen of the United States, a permanent resident, or a legal alien, in need of medical treatment or insurance, and have a low or very low income in order to qualify for Colorado Medicaid. Additionally, you must meet one of the prerequisites below:
- Pregnant, or
- Having parental responsibility for a kid under the age of 18
- Have a disability yourself or a family member who is disabled.
Annual Household Income Limits (before taxes)
| Household Size* | Maximum Income Level (Per Year) |
| 1 | $18,075 |
| 2 | $24,353 |
| 3 | $30,630 |
| 4 | $36,908 |
| 5 | $43,186 |
| 6 | $49,463 |
| 7 | $55,741 |
| 8 | $62,018 |
*For households with eight or more members, add $6,277 for each additional person.
Similar Articles:
- How to Get Florida Medicaid Benefits
- How to Get Kentucky Medicaid Benefits
- How to Get Georgia Medicaid Benefits | Best Answers
How do I contact Medicaid in Colorado?
Phone
303-866-2993
Website
- healthfirstcolorado.com
- Member Frequently Asked Questions | Colorado Department of Health Care Policy & Financing
- Basic Health Program | Medicaid
What are the Medicaid plans in Colorado?
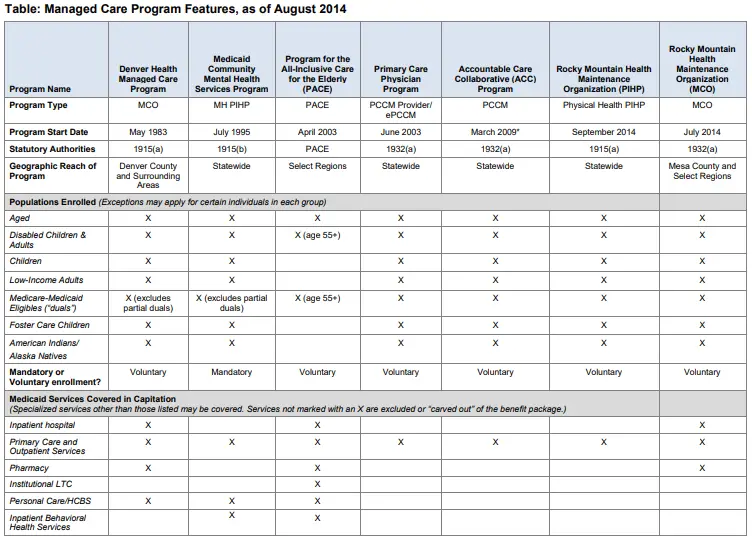
For the provision of services for its MCO program, the state has agreements with two regional nonprofit plans (Risk-based managed care organization Denver Health Medicaid Choice and one limited benefit prepaid health plan, Rocky Mountain HMO).
Keep in mind that each plan’s accessibility differs by location.
Additionally, the state has agreements with five behavioral health organizations to deliver mental health services in particular regions.
These organizations are Northeast Behavioral Health Partnership, Foothills Behavioral Health Partners, Colorado Health Partnerships, Behavioral Healthcare, Inc., and Access Behavioral Care.
For more than three decades, Colorado has utilized the MCO and PCCM managed care delivery models.
- Medicaid beneficiaries in Denver County and the surrounding areas can get acute, primary, and specialized treatment through the Managed Care Organization (MCO) program.
- The majority of Medicaid clients in the state are required to participate in the Medicaid Community Mental Health Care program, a mental health prepaid plan, which manages behavioral health services.
- The majority of Medicaid clients in the state who are not institutionalized can access the Primary Care Physician Program (PCPP).
- In some regions, beneficiaries who are elderly (age 55+) and have impairments and satisfy the criteria for nursing home level of care are eligible for the Program for All-Inclusive Care for the Elderly (PACE) program, which offers a variety of services, including Medicare and Medicaid Services.
- Most Medicaid clients in the state are served by the PCCM program known as Accountable Care Collaborative (ACC), which works with a network of Regional Care Collaborative Organizations (RCCOs) to coordinate acute, general, and specialty care, pharmacy, and some behavioral health services.
Similar Articles:
- How to Get Hawaii Medicaid Benefits | Best Answers
- How to Get Indiana Medicaid Benefits | Best Answers
- How to Get Iowa Medicaid Benefits | Best Answers
How do I apply for Colorado Medicaid?
Visit the Colorado PEAK online application page to submit an online application.
Visit the How to Apply page for further details on the application process. An application form will be available for direct download from the website.
Additionally, you can use the Marketplace application to see whether you are eligible.
What is covered by Colorado Medicaid?
The following services are covered by Colorado Medicaid
| Ambulance services | Organ & transplants |
| Behavioral health | Outpatient hospital services |
| Dental services | Physical, occupational, or speech therapy |
| Emergency room | Prescription drugs |
| Family planning | Preventive and wellness services |
| Home health | Provider visits |
| Hospice | Radiation therapy |
| Immunizations | Specialist visits |
| Laboratory services | Substance use treatment |
| Maternity & newborn care | Telemedicine |
| Mental health services | Urgent care centers |
| Non-emergency medical transportation | Vision care |
Copayments?
There is a charge for some of the services provided by Health First Colorado, Colorado’s Medicaid program. Copays are monetary payments that some members are required to give their provider in order to access specific services.
| Hospital services | $10 |
| Outpatient surgery | $0 |
| Outpatient emergency for non-emergency | $6 |
| Outpatient hospital services | $4 |
| Primary Care Physician and specialist services | $2 |
| Clinic services | $2 |
| Laboratory services | $1 |
| Radiology services | $1 |
| Prescription drugs | $3 |
What is Colorado Medicaid’s Copay Maximum?
The maximum copay per month for Health First Colorado members exists. This means that if a member has paid their monthly copay obligation up to a set amount, they are free from further copay obligations for the remainder of the month.
The formula used to determine this cap is 5% of the member’s monthly household income.
For instance, a family earning $900 per month would only have to pay $45 in copays for that month.
Can I have both Colorado Medicaid and Medicare?
An individual may be qualified for both Medicaid and Medicare and be able to take use of both programs simultaneously.
Medicaid, however, is usually paid last. You must use Medicare now that you are qualified for Medicare under Health First Colorado, Colorado’s Medicaid program.
Similar Articles:
- How to Get Kansas Medicaid Benefits | Best Answers
- How to Get Louisiana Medicaid Benefits
- How to Get Maine Medicaid Benefits
Is there a Medicaid waiver program in Colorado?
Twelve Medicaid waiver programs are available in Colorado, four of which are designed exclusively for people with intellectual and/or developmental impairments.
- *WAIVER for PERSONS with DEVELOPMENTAL DISABILITIES (formerly known as “comprehensive services”) (HCBS-DD)
- *SUPPORTED LIVING SERVICES WAIVER (HCBS-SLS)
- *CHILDREN WITH AUTISM WAIVER (HCBS-CWA)
- *CHILDREN’S EXTENSIVE SUPPORT WAIVER (HCBS-CES)
- CHILDREN’S HABILITATION RESIDENTIAL PROGRAM WAIVER (HCBS-CHRP)
- CHILDREN’S HCBS WAIVER (CHCBS)
- HCBS WAIVER for PERSONS with BRAIN INJURY (HCBS-BI)
- HCBS WAIVER for Community Mental Health Supports (HCBS-CMHS)
- HCBS WAIVER for PERSONS LIVING WITH AIDS (HCBS-PLWA)
- HCBS WAIVER for PERSONS who are ELDERLY, BLIND, AND DISABLED (HCBS-EBD)
- HCBS Waiver for Children with Life-Limiting Illness (HCBS-CLLI)
- HCBS waiver for persons with Spinal Cord Injury (pilot) (HCBS-SCI)
What programs assist people who have developmental disabilities?
Adults with developmental impairments in Colorado are helped by the waiver for persons with developmental disabilities and the waiver for assisted living services.
Colorado offers assistance to kids with developmental problems through the HCBS children with autism and the children’s extended support waiver.
What is the best Medicaid in Colorado?
Denver Health Medicaid Choice and Rocky Mountain Health Plans Prime are the two managed care programs offered by Health First Colorado, Colorado’s Medicaid program.
What is the highest income limit for Colorado Medicaid?
In Colorado, the monthly income cap for Medicaid HCBS is $2,349 for single individuals and $4,698 for married individuals (and both spouses are applying). In Colorado in 2020, spousal impoverishment regulations may raise a non-applying spouse’s monthly income by $2,155 to $3,216.
Will you still have Colorado Medicaid once you are over 18?
If you’re 19 or older, Health First Colorado (Medicaid) is available. If you are 19 years of age or older and meet the following criteria, you may be eligible for Health First Colorado (Medicaid): You have a low income, whether or not you have a disability; or. You are disabled, underfunded, and have a low income.
What documents do I need to apply for Medicaid?
Copies of the following documentation must be submitted with your Medicaid application in order to establish your eligibility. Your application’s processing time will go faster as a result. Medicaid considers your eligibility as a couple if you are married or in a domestic partnership.
Even if they are not in need of services or you are not living together, you must include the following information for anyone to whom you are legally married.
- Driver’s license or other photo ID, passport, birth certificate, or immigration documents are acceptable forms of identification.
- Medicare card as well as any other health insurance cards, such as Medicare Advantage or prescription medication cards
- A copy of your Social Security statement (you can print your statement here and register for a Social Security online account: https://www.ssa.gov/myaccount/)
- Proof of any other retirement or pension income received; the statements supplied must show the gross amount of the pension or retirement account.
- A letter outlining any deposits or withdrawals above $500 that aren’t marked with the depositor’s or receiver’s name; copies of your three (3) most recent months’ worth of bank statements from each of your checking and savings accounts.
- Copies of the financial durable power of attorney and the medical durable power of attorney
- Evidence of expenses, such as utility bills, rent or property taxes, or medical charges
- If you have bought a burial or funeral coverage, a copy of the prepaid/irrevocable document is required
- A copy of the life insurance policy with the current cash value statement
- A copy of financial securities
- Vehicle registration copy
