This article is a collection of the best answers to Indiana Medicaid’s most frequently asked questions.
Medicaid is a government-sponsored healthcare program for low-income families and individuals who fulfill specific income and resource requirements. Only the aged, blind, or disabled can access resources within the defined restrictions.
We have scoured the internet to provide all you need to know about the Indiana Medicaid Benefits.
You will learn everything you need to know about Indiana Medicaid in this article.
Table of Contents
What is the Indiana Medicaid Program?
Under the auspices of Indiana Health Coverage Programs, Indiana Medicaid offers a healthcare safety net to Hoosier children, the elderly, the disabled, pregnant women, and other qualified groups (IHCP). A health insurance program for eligible adults aged 19 to 64 is called the Healthy Indiana Plan.
Who is eligible for Indiana Medicaid?
You must be a resident of Indiana, a national or citizen of the United States, a permanent resident, or a legal alien needing health care or insurance help, and have a low income to qualify for Indiana Medicaid. The Healthy Indiana Plan will provide coverage for most non-disabled persons (HIP).
People with disabilities or those residing in institutions certified by Medicaid may be subject to higher income and asset restrictions.
Based on family size and income, several categories demand the payment of a monthly premium or contribution.
A family’s income will be reduced to 5% of the yearly Federal Poverty Limit for the Healthy Indiana Plan.
Annual Household Income Limits (before taxes)
| Household Size* | Maximum Income Level (Per Year) |
| 1 | $16,971 |
| 2 | $22,930 |
| 3 | $28,888 |
| 4 | $34,846 |
| 5 | $40,805 |
| 6 | $46,763 |
| 7 | $52,722 |
| 8 | $58,680 |
*For households with more than eight members, add $5,958 per additional person.
Similar Articles:
- How to Get Kansas Medicaid Benefits | Best Answers
- How to Get Louisiana Medicaid Benefits
- How to Get Maine Medicaid Benefits
How do I contact Medicaid in Indiana?
Phone
1-800-403-0864
Website
What are the Medicaid plans in Indiana?
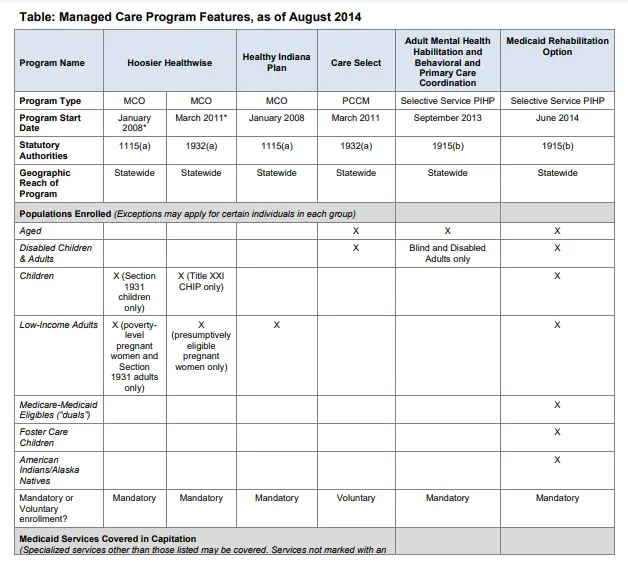
For Hoosier Healthwise and the Healthy Indiana Plan, Indiana has contracts with two national, for-profit plans (Anthem and Managed Health Services, owned by Centene) and one locally-based, non-profit plan (MDwise).
Using competitive bids within price ranges, the state establishes rates and chooses plans through a competitive procurement process. The Indiana Comprehensive Health Insurance Association (ICHIA), via Xerox, oversees the HIP’s Enhanced Services Plan on a fee-for-service basis.
Indiana has agreements with two care management organizations, or CMOS, for the Care Select program (Advantage Health Solutions and MDwise).
- Hoosier Healthwise (HHW) is a comprehensive risk-based managed care program for pregnant women, children, and parents.
- Adults who make less than 200 percent of the federal poverty line must enroll in the Healthy Indiana Plan (HIP), a statewide, comprehensive risk-based managed care program. HIP covers acute, primary, specialty, and behavioral health services; pharmacy benefits are excluded from the benefit package.
- The optional Care Select PCCM program in Indiana was started in 2008. Members with a specific chronic ailment (such as asthma, diabetes, or severe mental illness) who also meet other eligibility requirements can access it statewide (aged, blind, disabled, foster children, or children receiving adoptive services).
What is covered by Indiana Medicaid?
The following services are covered by Indiana Medicaid
| Chiropractic services | Mental health care |
| Clinic services | Non-emergency transportation |
| Dental care | Nursing facility services |
| Doctor visits | Over-the-counter drugs |
| Emergency transportation | Physical and occupational therapy |
| Family planning services | Podiatry Services |
| Home health care | Prescription drugs |
| Hospice care | Substance abuse services |
| Hospital care | Vision care |
| Lab and X-ray services | Well-child visits |
| Medical supplies and equipment | Wellness visit |
Copaypayments?
| Traditional Medicaid | Hoosier Care Connect | Hoosier Healthwise (Package C-only) | |
| Non-Emergency Transportation | $0.50 – $2.00 | $1 (each way) | Non-covered |
| Emergency Transportation | No copay | No copay | $10.00 |
| Pharmacy (Generic) | $3.00 | $3.00 | $3.00 |
| Pharmacy (Brand Name) | $3.00 | $3.00 | $10.00 |
| Non-emergency use of ER | No copay | $3.00 | No copay |
Similar Articles:
- How to Get Maryland Medicaid Benefits
- How to Get Massachusetts Medicaid Benefits
- How to Get Michigan Medicaid Benefits
Depending on your plan, the following copays may also apply:
| Non-Preventive Physician Visit | $4 |
| Non-Emergency Use of ER | $8 |
| Inpatient Hospital Visit | $75 |
What is not covered by Copay?
Copays do not apply to:
- Members who are pregnant
- Members of Native American descent
- Members who have exhausted their 5% cost-sharing cap
- Maternity services
- Family planning services
- Preventive care services
Can I have both Indiana Medicaid and Medicare?
An individual may be qualified for both Medicaid and Medicare and be able to use both programs simultaneously. “Dual eligibles” or occasionally “Medicare-Medicaid enrollees” are those who qualify for both Medicare and Medicaid.
People must be enrolled in Medicare Part A (hospital insurance) and Medicare Part B to be considered dual eligible (medical insurance).
What is the highest income limit for Indiana Medicaid?
The highest income limit for a household size of one is $16,971. A family’s income will be reduced to 5% of the yearly Federal Poverty Limit for the Healthy Indiana Plan.
What are the different types of Medicaid in Indiana?
The following healthcare programs included under the Indiana Health Coverage Programs (IHCP) umbrella are the primary programs serving most children and adults, as well as those designed to serve special member populations.
- IHCP Programs and Services
- Healthy Indiana Plan (HIP)
- Hoosier Care Connect
- Hoosier Healthwise
- Traditional Medicaid
- Home- and Community-Based Services (HCBS)
- Aged and Disabled Waiver Program
- Community Integration and Habilitation Waiver Program
- Family Supports Waiver Program
- Traumatic Brain Injury Waiver Program
- Adult Mental Health Habilitation Program
- Behavioral and Primary Healthcare Coordination Program
- Child Mental Health Wraparound Program
- Program for All-Inclusive Care to the Elderly (PACE)
- Family Planning Eligibility Program
- 590 Program
- Medicare Savings Programs
- HoosierRx
What documents do I need to apply for Medicaid?
You may need one or more of the following information to complete your application, whether you’re applying for the first time or renewing your benefits:
- Everyone requesting benefits must provide proof of citizenship and identity.
- If you have non-U.S. citizens in your family, you’ll need Alien Registration Cards.
- Everyone should have a Social Security number or proof that one has been applied for.
- Everyone claiming benefits should have a copy of their birth certificate.
- The name, address, and daytime phone number of the landlord or neighbor
- A statement that verifies your residence and the names of all people who live with you. A non-relative who does not live with you must make the assertion. It must be signed, dated, and contain the person’s name, address, and phone number.
- Proof of ALL money your household got last month and this month from whatever source.
- Proof confirming your employment ended and that you were paid till the end of the month.
- Any other medical insurance must be verified.
How much money can you have in the bank on Indiana Medicaid?
You can only have a certain number of resources and be eligible for Medicaid. A single person may only spend $1,500, while a married couple may spend $2,250. Land, money, bank accounts, insurance policies, and some vehicles are examples of resources.
Similar Articles:
- How to Get Minnesota Medicaid Benefits
- How to Get Mississippi Medicaid Benefits
- How to Get Missouri Medicaid Benefits
Does the disabled person get Indiana Medicaid?
Indiana Medicaid offers coverage to the elderly, blind, and crippled through two programs. By clicking on the links below, you can find out more about each program:
- Traditional Medicaid – about those who qualify for home and community-based services
- Hoosier Care Connect – for the majority of elderly, blind, and disabled people who qualify for coverage
Will you still have Indiana Medicaid once you are over 18?
The Affordable Care Act’s 2010 passage is one source of assistance. The legal age limit for staying on a parent’s health insurance plan after turning 18 is 26.
What is the best Medicaid in Indiana?
MDwise is the top-ranked Indiana Medicaid health plan with a score of 82.2 percent, up from the previous year. Out of 213 Medicaid plans across the US, the company came in at position 45.
