Understanding medicaid eligibility for children can feel overwhelming for parents. You want to ensure your kids get quality healthcare coverage. Over 37 million children nationwide receive Medicaid or CHIP benefits. Medicaid provides comprehensive health insurance for children from birth through age 18. Income limits vary by state but remain generous nationwide.
Your children may still qualify, even if you earn a decent income. This guide explains everything about medicaid eligibility age 0-18 requirements nationwide. You’ll learn how to apply Medicaid for children under 18 successfully. We cover state medicaid income limits for kids across all 50 states. You’ll discover the medicaid eligibility child poverty level standards for 2026.
We also explain the eligibility pathways for medically needy Medicaid children in full detail. Plus, you’ll understand Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefits. By the end, you’ll know exactly how to get coverage. Let’s start with the basics and build your knowledge systematically.
Table of Contents
Understanding Medicaid for Children: The Basics

Medicaid is the most extensive health insurance program in America for low-income families. The federal government partners with your state to fund Medicaid programs. However, your state administers the program and sets specific eligibility rules. Children represent nearly half of all Medicaid beneficiaries in America.
Understanding medicaid eligibility for children starts with knowing what programs exist. Both Medicaid and the Children’s Health Insurance Program (CHIP) serve children. Together, these programs create a safety net for uninsured children. According to Healthcare.gov, these programs ensure that children receive the necessary health services.
What Does Medicaid Cover for Your Children?
Your children receive comprehensive healthcare services through Medicaid or CHIP programs. Coverage includes doctor visits, hospital stays, and emergency room care on a daily basis. Prescription medications and immunizations are fully covered without any copays. Mental health services and substance use disorder treatment are included.
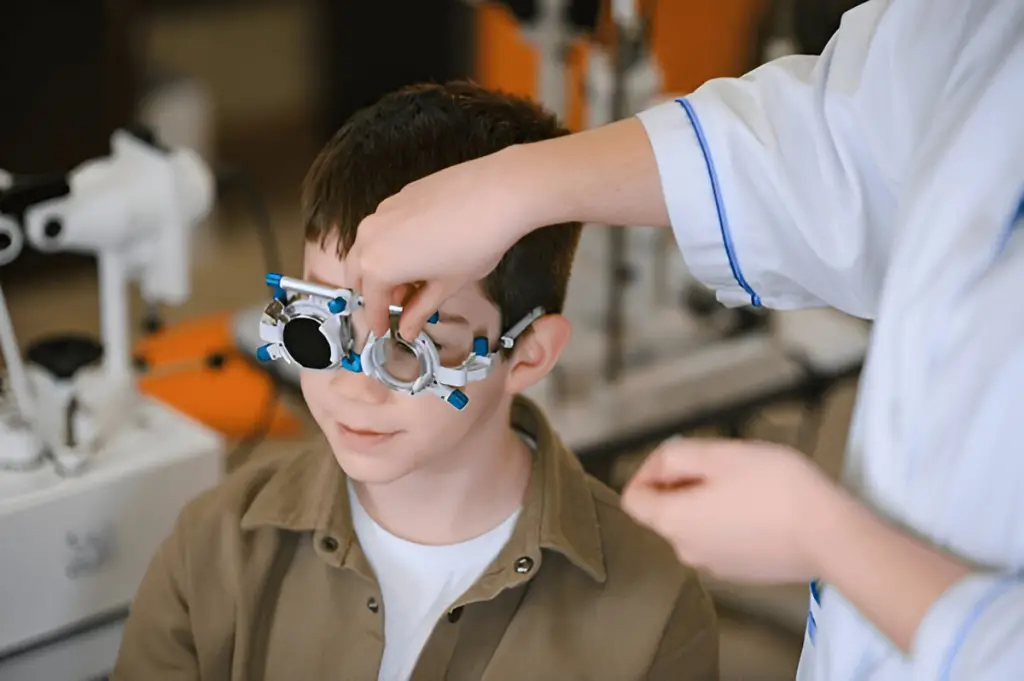
Vision services provide eyeglasses and eye exams for your children. Dental care covers checkups, cleanings, fillings, and necessary dental treatments. Laboratory tests and X-rays are covered when medically needed.
Medicaid vs CHIP: Understanding the Difference
Medicaid and CHIP work together to effectively cover uninsured children. Medicaid serves children in families with lower annual income levels. CHIP covers children whose family income exceeds Medicaid eligibility limits. Some states combine both programs under one name and system. Other states run separate Medicaid and CHIP programs for families.
Both programs provide similar comprehensive coverage for your children ages 0-18. You can apply for both programs through the same application. Your state determines which program is automatically available to your family based on your income. The transition between programs occurs automatically based on changes in income.
Federal Poverty Level and Income Requirements Explained

The Federal Poverty Level (FPL) determines Medicaid eligibility for children nationwide based on their poverty level. The Department of Health and Human Services updates FPL guidelines annually. For 2026, understanding FPL is crucial for the success of your application.
Federal minimum standards require states to cover specific groups of children. States must cover children up to at least 154% FPL. However, most states expand coverage well beyond this minimum requirement.
2026 Federal Poverty Level Guidelines
Your family size determines your applicable Federal Poverty Level amount. Here are the 2026 FPL guidelines for the contiguous 48 states:
| Family Size | Annual Income | Monthly Income |
| 1 person | $15,650 | $1,304 |
| 2 persons | $21,150 | $1,763 |
| 3 persons | $26,650 | $2,221 |
| 4 persons | $32,150 | $2,679 |
| 5 persons | $37,650 | $3,138 |
| 6 persons | $43,150 | $3,596 |
| 7 persons | $48,650 | $4,054 |
| 8 persons | $54,150 | $4,513 |
For each additional person beyond 8, an additional $5,500 is charged annually, or $458 monthly. Alaska and Hawaii have higher FPL amounts due to living costs.
Understanding Modified Adjusted Gross Income (MAGI)
Medicaid uses Modified Adjusted Gross Income (MAGI) to determine eligibility. MAGI includes your wages, salaries, and self-employment income combined. It also includes Social Security benefits, pensions, and investment income. However, MAGI excludes certain types of income from the calculation entirely.
The 5% income disregard automatically increases your eligibility threshold slightly. This means your countable income is reduced before comparison. This helps more families qualify for needed medical coverage services.
Age-Based Eligibility Categories: Birth Through Age 18

Medicaid eligibility for individuals aged 0-18 varies significantly by age group. States typically use three main age categories for children. Understanding these categories helps you know your child’s eligibility chances.
Infants Under Age 1: Highest Income Limits
Infants receive the most generous income limits under Medicaid. Most states cover infants up to 200-300% of FPL. Some states even reach up to 317% FPL for infants. This ensures newborns get critical early healthcare without barriers.
If your baby’s mother had Medicaid during pregnancy, automatic coverage applies. Your newborn receives guaranteed coverage for 12 full months. You don’t need to submit a separate application initially. However, you should still complete enrollment paperwork to continue coverage.
Young Children Ages 1-5: Moderate Income Limits
Children ages 1 through 5 typically qualify up to 154% FPL. Many states exceed this minimum and cover up to 200% FPL. Some generous states reach 300% FPL for young children. This ensures preschoolers receive preventive care and developmental screening services.
Continuous eligibility policies protect young children from coverage gaps. Your child cannot lose coverage mid-year except for specific reasons. Moving out of state or gaining other insurance are exceptions.
School-Age Children Ages 6-18: Standard Limits
Children ages 6 through 18 typically qualify up to 154% FPL. However, CHIP extends coverage up to 200-400% FPL, usually. This ensures that school-age children maintain access to healthcare throughout their childhood years.
Coverage typically ends when your child turns 19 years old. Some states extend coverage through age 20 for students. Former foster care youth can maintain coverage through age 26.
Complete 50-State Income Limits for Children’s Medicaid and CHIP
Understanding state medicaid income limits kids requires knowing your specific state. Each state sets income limits as a percentage of FPL. The table below shows medicaid eligibility for children across America.
Data is sourced from the Centers for Medicare & Medicaid Services official eligibility tables. These represent the most current information available for 2026.
Medicaid and CHIP Income Eligibility by State (2026)
| State | Medicaid Children Ages 0-1 (% FPL) | Medicaid Children Ages 1-18 (% FPL) | CHIP Maximum (% FPL) |
| Alabama | 146% | 146% | 317% |
| Alaska | 213% | 175% | 213% |
| Arizona | 147% | 147% | 200% |
| Arkansas | 214% | 214% | 214% |
| California | 266% | 266% | 317% |
| Colorado | 268% | 268% | 268% |
| Connecticut | 201% | 201% | 323% |
| Delaware | 212% | 212% | 212% |
| District of Columbia | 324% | 324% | 324% |
| Florida | 213% | 210% | 213% |
| Georgia | 215% | 215% | 250% |
| Hawaii | 201% | 201% | 326% |
| Idaho | 190% | 190% | 190% |
| Illinois | 213% | 213% | 318% |
| Indiana | 213% | 213% | 266% |
| Iowa | 380% | 380% | 380% |
| Kansas | 246% | 246% | 246% |
| Kentucky | 213% | 213% | 213% |
| Louisiana | 211% | 211% | 250% |
| Maine | 213% | 213% | 213% |
| Maryland | 264% | 264% | 324% |
| Massachusetts | 210% | 210% | 310% |
| Michigan | 215% | 215% | 222% |
| Minnesota | 288% | 288% | 288% |
| Mississippi | 211% | 211% | 211% |
| Missouri | 215% | 215% | 305% |
| Montana | 276% | 276% | 276% |
| Nebraska | 215% | 215% | 215% |
| Nevada | 205% | 205% | 205% |
| New Hampshire | 213% | 213% | 318% |
| New Jersey | 213% | 213% | 355% |
| New Mexico | 241% | 241% | 355% |
| New York | 223% | 223% | 405% |
| North Carolina | 216% | 216% | 216% |
| North Dakota | 185% | 185% | 185% |
| Ohio | 213% | 213% | 318% |
| Oklahoma | 215% | 215% | 215% |
| Oregon | 210% | 210% | 320% |
| Pennsylvania | 220% | 220% | 325% |
| Rhode Island | 266% | 266% | 266% |
| South Carolina | 216% | 216% | 216% |
| South Dakota | 214% | 214% | 214% |
| Tennessee | 215% | 215% | 250% |
| Texas | 209% | 209% | 209% |
| Utah | 210% | 210% | 210% |
| Vermont | 321% | 321% | 321% |
| Virginia | 215% | 215% | 215% |
| Washington | 322% | 322% | 322% |
| West Virginia | 214% | 214% | 319% |
| Wisconsin | 308% | 308% | 308% |
| Wyoming | 213% | 213% | 213% |
Note: All percentages include the automatic 5% income disregard. Data sourced from Medicaid.gov.
State-Specific Highlights and Variations
Several states offer exceptionally generous coverage for children overall. New York provides CHIP coverage up to 405% FPL. Iowa covers children up to 380% FPL through Medicaid. District of Columbia and Washington state both exceed 320% FPL. Vermont’s program reaches 321% FPL for all children.
Conversely, some states maintain closer to federal minimum requirements. North Dakota covers children up to 185% FPL only. Idaho’s program reaches 190% FPL for children statewide. Texas covers children up to 209% FPL through Medicaid.
The Medically Needy Pathway for Children

The medically needy medicaid children eligibility pathway helps families financially. Your family might earn too much for regular Medicaid coverage. However, high medical expenses can still qualify your children. This pathway is commonly referred to as “spend-down” in many states.
How the Medically Needy Program Works
Medically needy programs consider your medical bills in conjunction with your income. You calculate your excess income above the Medicaid limit. Then, you subtract unreimbursed medical expenses from your excess income. If medical bills reduce your income below limits, you qualify.
For example, your family earns $3,500 monthly with four members. Your state’s Medicaid limit is $2,679 monthly for families. Your excess income is $821 per month above limits. However, your child has $1,000 monthly in medical expenses. After subtracting medical costs, you’re below the income limit. Your child now qualifies through the medically needy pathway.
Which States Offer Medically Needy Programs
Currently, 33 states, plus Washington, D.C., operate medically needy programs. Children and pregnant women must be included in these programs. According to Medicaid.gov, the following states offer medically needy pathways:
States with Medically Needy Programs: Arkansas, California, Connecticut, Delaware, District of Columbia, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nebraska, New Hampshire, New Jersey, New York, North Carolina, North Dakota, Pennsylvania, Rhode Island, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, and Wisconsin.
If your state isn’t listed, other pathways might exist. Contact your state Medicaid office to explore all options available.
Calculating Your Medically Needy Income Limit (MNIL)
Each state sets its own medically needy income limit (MNIL). The MNIL is usually lower than regular Medicaid limits. Your medical bills must bring income below this MNIL level. Check your state’s Department of Health or Department of Human Services website. They provide specific MNIL amounts for your family size.
EPSDT: Early and Periodic Screening, Diagnostic, and Treatment

EPSDT is a comprehensive child health program within Medicaid. Every child enrolled in Medicaid automatically receives EPSDT benefits. This program ensures children get preventive care and treatments. Understanding EPSDT helps you maximize your child’s healthcare coverage.
What EPSDT Covers for Your Children
EPSDT provides much broader coverage than adult Medicaid services. Your children receive comprehensive health and developmental services on a regular basis. Screenings include physical examinations, vision tests, and hearing evaluations.
Developmental assessments ensure your child meets age-appropriate milestones adequately. Dental screenings catch problems early before they become serious.
If screening identifies any problems, Medicaid must cover treatment. Treatment includes any medically necessary service to correct problems. This applies even if your state doesn’t cover that service for adults. Your child’s needs take priority under EPSDT federal requirements.
Screening Schedule and Preventive Care
EPSDT requires regular well-child visits throughout a child’s development. Infants receive multiple checkups during the first year alone. Young children get annual screenings to monitor growth and development. School-age children continue receiving yearly comprehensive physical examinations.
Immunizations follow the Centers for Disease Control and Prevention recommended schedule. All vaccines are provided at no cost to you. Vision and hearing tests are typically performed at specific ages automatically. Dental checkups usually begin when teeth first appear.
Treatment Services Under EPSDT
EPSDT treatment includes any medically necessary service for children. Physical therapy helps children with movement or coordination problems. Speech therapy addresses communication and language development delays thoroughly.
Occupational therapy teaches skills for daily living activities. Mental health services include counseling, treatment, and psychiatric medications.
Medical equipment, such as wheelchairs, braces, and hearing aids, is covered. Home health services bring care directly to your home. Durable medical equipment ensures your child has the necessary tools. All treatments must correct or ameliorate the identified conditions.
How to Apply Medicaid for Children Under 18

Applying for medicaid eligibility for children is straightforward with guidance. Multiple application methods exist to accommodate different family preferences. You can apply online, by phone, by mail, or in person. Select the process that is most convenient for your current situation.
Required Documentation for Your Application
Gather necessary documents before starting your application process. You’ll need proof of your child’s age and identity. Birth certificates are most effective for proving age requirements. Social Security numbers are required for all household members. Proof of income includes recent pay stubs or tax returns.
If you’re self-employed, provide your business income records. Bank statements show your financial account information clearly. Proof of residency includes utility bills or lease agreements. Citizenship or immigration documents prove your child’s legal status.
Step-by-Step Application Process
Step 1: Choose Your Application Method
Visit Healthcare.gov to apply for Medicaid/CHIP online. Alternatively, you can visit your state’s Medicaid website directly to apply. You can also contact your state’s Medicaid hotline for assistance. Some families prefer applying in person at local Medicaid offices.
Step 2: Create an Account or Start Application
Online applications require creating a secure account with a password. Provide your email address and basic contact information initially. Answer questions about your household size and composition accurately. Include all children currently living in your home.
Step 3: Provide Income Information
Report all sources of income your household receives regularly. Include wages, self-employment, Social Security, and child support payments. Be honest and accurate about your monthly income amounts. Underreporting can delay your application or cause problems later.
Step 4: Submit Required Documentation
Upload or mail copies of the required documents to the authorities. Never send original documents unless specifically requested by staff. Keep copies of all submissions for your records. This protects you if documents get lost during processing.
Step 5: Wait for Eligibility Determination
Your state has 45 days to process most applications. Disability-related applications may take up to 90 days maximum. You’ll receive a written notice of the decision made. Approved applications include your child’s Medicaid identification card.
Common Application Mistakes to Avoid
Many applications get delayed due to preventable mistakes families make. Failing to sign the application is a common oversight problem. Failing to include Social Security numbers results in immediate delays. Providing outdated income information leads to incorrect eligibility determinations.
Missing documentation is the most frequent application problem encountered. Check your state’s requirements carefully before submitting all necessary documents. Incomplete applications remain in pending status until they are completed fully. Follow up regularly if you don’t hear back within the timeframes.
Presumptive Eligibility: Getting Immediate Coverage
Presumptive eligibility provides temporary Medicaid coverage while the application is being processed. Qualified entities can determine presumptive eligibility on the spot. Hospitals, community health centers, and clinics often provide this service. Your child receives immediate coverage for the outpatient services provided.
Presumptive eligibility typically lasts 60 days or until a determination is made. You must still complete a full application during this time. This protects children needing immediate medical care while awaiting decisions.
Enrollment Barriers and Tips for Success

Understanding common enrollment barriers helps you navigate the system. Many families face challenges during the application process. Knowing these obstacles in advance enables you to prepare better.
Language and Communication Barriers
Language differences can complicate the application process for families. Most states now provide applications in multiple languages. Spanish translations are widely available across all 50 states. Other languages depend on your state’s population needs.
Request interpreter services if you’re not fluent in English. Phone interpretation is available during calls to Medicaid offices. In-person appointments can also include qualified medical interpreters. Don’t let language barriers prevent your children from coverage.
Document Collection Challenges
Gathering required documents proves difficult for some families, unfortunately. Birth certificates might be from other states or countries. Obtaining copies involves time, money, and effort on your part. Immigration documents may be in processing or temporarily unavailable.
Begin collecting documents early, before you need to apply. Contact the vital records office to order a certified birth certificate. Request Social Security cards from the Social Security Administration promptly. Many documents can be requested online for convenience.
Understanding Complex Income Rules
The income calculation often confuses many applicants during the process. Understanding what counts as income requires an understanding of MAGI rules. Some income types are excluded from consideration entirely.
Tax returns help determine your Modified Adjusted Gross Income. However, recent income changes may not be reflected in returns. Provide current pay stubs showing your actual earnings now. Explain any income fluctuations in your application notes clearly.
Addressing Application Denials
If your application is denied, don’t give up hope. You have the right to appeal any denial decision. Appeal deadlines are typically 60 to 90 days maximum. Read your denial notice carefully to understand the reason for the denial.
Common reasons for denial include incomplete applications or missing documentation. Income calculation errors happen frequently and are easily corrected. Reapply with corrected information or request a fair hearing. Many denials are overturned when families provide additional information.
Tips for Maintaining Continuous Coverage
Once your child has coverage, maintaining eligibility is essential. Report income changes within 10 days to your state. Update your address to ensure you receive renewal notices. Respond promptly to all requests for information.
Annual redetermination requires submitting updated information to the authorities on an annual basis. Don’t miss renewal deadlines, or coverage will terminate automatically. Set reminders for important dates to avoid lapses. Keep copies of all submissions for your records permanently.
Frequently Asked Questions (FAQs)
Q1: Can my children get Medicaid if I don’t qualify?
Yes, children’s Medicaid eligibility is determined separately for children. Your children can qualify even if you earn too much. Children’s income limits are significantly higher than those for adults. Apply for your children regardless of your own income.
Q2: Do assets affect my child’s Medicaid eligibility?
No, most states don’t count assets for children’s Medicaid. Only income matters for Medicaid eligibility, specifically for the age 0-18 determination. Bank accounts, vehicles, and homes typically do not affect eligibility. Focus on meeting income requirements without worrying about assets.
Q3: What happens if my income changes after approval?
Report income changes to your state Medicaid office within 10 days. Your child’s eligibility might change based on new income. If your income decreases, your child remains eligible without any issues. If income increases, your child might transition to CHIP coverage.
Q4: Can immigrant children qualify for Medicaid coverage?
Yes, lawfully present immigrant children can qualify for Medicaid. Citizenship requirements depend on your state’s specific policies. Many states cover all legally residing children regardless. Emergency Medicaid covers all children for emergency services only.
Conclusion
Understanding medicaid eligibility for children ensures your kids get healthcare. Income limits vary significantly across all 50 states. Most children in families earning up to 200-400% FPL qualify. The medically needy pathway helps families with high medical costs.
EPSDT benefits provide comprehensive preventive and treatment services automatically. Apply Medicaid for children under 18 through Healthcare.gov or your state. Don’t let perceived barriers prevent you from applying today. Your children deserve quality healthcare coverage regardless of income. Start your application now and secure your child’s health.
